Constipation in the elderly with dementia isn’t pleasant to have or talk about. However, if it’s not treated, it could lead to more severe conditions or be a sign of another illness.
We’ve been dealing with constipation issues for my mum with Alzheimer’s for years. Maintaining the correct equilibrium of conditions is challenging to ensure that mum doesn’t become constipated or, in some cases, go the other way and experience diarrhoea.
**if you do suffer from chronic constipation, your first port of call should always be your doctor, especially if you see a significant difference in frequency, colour, have pain or notice blood in your bowel movements**
What is Constipation?
You can see if someone is constipated if they infrequently defecate (less than 2-3 times) a week, pass hard stools, strain to use the toilet, or do not feel like they’ve evacuated.
Constipation is a symptom of some untreated issue with your body. When it becomes chronic, it can lead to increased pain, internal problems, depression and worsening quality of life.
Constipation is more prevalent in the elderly & women, and it’s estimated that 1 in every 7 adults has constipation, the number increasing for those with dementia.
How Do You Know If An Elder With Dementia Is Constipated?
It can be challenging for someone with dementia to express that they have constipation. Look out for signs like they may be experiencing more confusion, pain, symptoms of discomfort, behavioural changes, or aggression that all can be mistaken for other issues,
It can get missed by health practitioners like UTIs, so knowing what to look out for and having tools to reduce chronic constipation are essential for caregivers.
We’re trying to avoid chronic constipation, which could develop into faecal impaction by forming hard, dry stools that block the colon/ rectum. It can also present with symptoms of faecal incontinence, as stool can’t be passed and a liquid overflow pushes through & can be mistaken as diarrhoea.
What Stool Consistency indicates Constipation in The Elderly With Dementia?
While frequency can be a guide, you can tell more directly by looking at your stool consistency. When you evacuate, you’re constipated if stools look like type 1 & 2 in this Bristol Stool chart. If you’re producing watery stools, you may be impacted. If you haven’t been able to go for over a week, it’s time to take steps like laxatives and talk to your doctor.
Here’s a handy guide by WebMD on different types of stools and explains what your stool’s colour and type mean.
Treat with Dignity, Respect, and avoid the Guilt
Everyone has the right to privacy, dignity and respect, which is why talking about embarrassing things like bowel movements can be very difficult to broach with your loved ones.
As dementia caregivers, we need to put on our detective caps and look for signs of any distress or monitor output before it becomes more severe and further interventions are required.
There are many reasons why the body’s ability to produce natural bowel movements can be interrupted. You all know the basics, eating healthy, drinking lots of water, exercising regularly, 5 portions of fruit & veg, getting enough fibre etc. all help with constipation.
But you might not know that stress, depression, medication, diabetes, Parkinson’s, IBS, spinal cord/ nerve damage, and weak pelvic floor can all impact constipation etc.
I remember feeling incredibly guilty that in helping mum follow all the guidance on encouraging regular bowel movements, she still became constipated despite my best efforts. After talking to our doctor, she explained all mom’s health issues and how her medication contributed to her constipation. If you’re concerned, get your doctor to review, they may see things other than diet/lifestyle causing constipation in the elderly with dementia.
What Specific Issues Can Cause Constipation In The Elderly With Dementia?
A couple of factors impact the elderly with dementia more than others, but it depends on their age and the severity of their dementia. The more severe dementia, the more likely that brain damage makes it harder for your loved one to understand the sensations triggered that signal the need for bowel movements.
Medications
For example, if your loved one is on opiates/NSAIDs that help reduce pain or antidepressants like Amitriptyline. Some elders suffer from arthritic pain and may be prescribed stronger pain meds to help deal with that. They make calcium supplements, antacids for reflux, iron supplements etc., all contribute to constipation and need to be mitigated.
Low fluid intake
They may be fearful of drinking too much to avoid incontinence accidents, simply find it difficult to remember how much liquid they’ve consumed during the day, or even lack that brain connection and simply don’t feel thirsty. A study in Taiwan of 119 dementia patients found that “low liquid consumption was the predictor of constipation among patients with dementia”
Mobility
Dementia can affect your mobility & your balance, which can make it more difficult to use a toilet. Your loved ones may need assistance with different options like a commode, bedpan or even incontinence pants.
Like my mother, who can’t walk, & is hoisted, then you’re more likely to suffer from constipation due to the lack of daily movement. In this case, talking with your GP may mean you will need chemical interventions like laxatives, common in the elderly if diet/water intake alone doesn’t help.
Taste
Taste may be challenging to include healthy snacks, dementia tends to favour sweet food, or food may taste bland or awful. Wendy Mitchell, with young onset dementia, has talked about how dementia affected her taste buds.
My tastebuds are another thing that have been affected. I used to love mushrooms with everything, now they don’t taste of anything…….My craving for sweet food has gone, in fact everything tastes doubly sweet, which is so off-putting.
Wendy Mitchel in “How dementia robbed me of my love of cooking” Observer
Line of Sight
If you can’t find the toilet or cannot distinguish it in the bathroom, you’re more likely to either hold it or have an accident in the wrong area. Using labels, marking and differentiating the toilet by colour from its surroundings will help when the urge strikes and fends off the start of constipation.
Routines
The most crucial thing with dementia is maintaining existing habits where possible. So if your loved one regularly uses the bathroom in the morning, then help encourage that as much as possible by reminding them it’s time to use the toilet or using signage to prompt them. Your bowel habits are your own. You may go as soon as you wake up, after meals, or in the evening. Stick to their habits unless constipation begins, and you may need to change your diet or add laxatives.
Bowel Diary
I advise all dementia caregivers to keep what I call a poo diary! I’d be lost without mine as the days merge. I’m thankful I did, as it is so much easier to notice patterns and give accurate factual information to your doctor about any changes for them to use in their diagnostic assessment.
Mum ranges from being constipated to having diarrhoea. She’s on laxatives, has suppositories, and I manage her diet.
Her issue is water intake and medication contributing to her constipation. Finding that sweet spot takes time, so a bowel diary is crucial to see when she last went and the type/consistency of stool. Great if you can add in what you eat, but I barely have time to register the bowel movement.
Keep it simple. Attached is the copy of my bowel movement chart that I started with, and then I just added the terminology to the daily family calendar rather than having a separate tool. The type refers to the Bristol Stool Chart. You can do it digitally or use paper copies. Whatever is easiest for you, and I happily discuss it with mum, so she understands the need, for example, a suppository at that time.
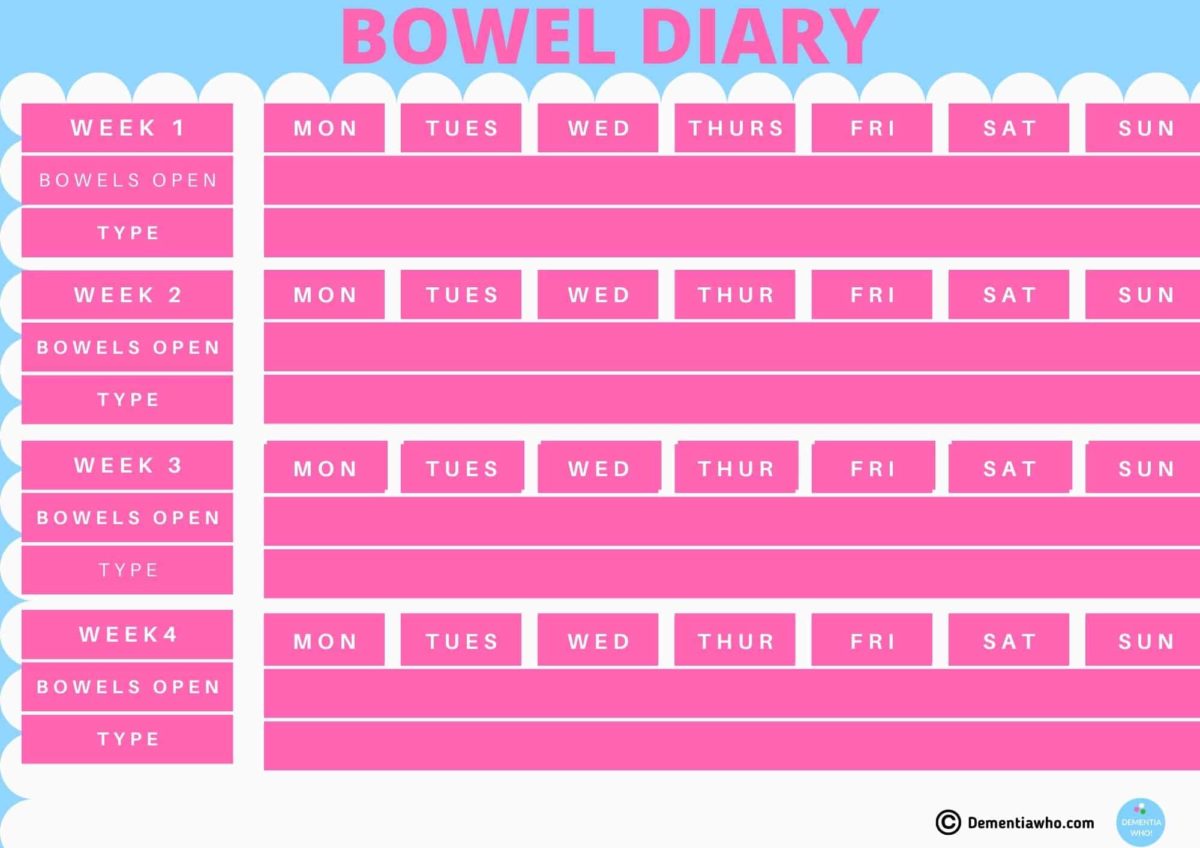
I know my mother’s bowel habits and stool consistency, shape, and colour, so I know when something is wrong. For those dementia caregivers reading this who haven’t had to deal with poo yet, you’ll be amazed how easily you get over your squeamishness, smell or have issues with dealing with clean up! Honestly!
I hope this article and anecdotal information, have helped explain a little more about the issues of constipation and dementia. Don’t be put off when it goes off-kilter. Review the situation again & see what needs changing.
Check out our next article, where we’ll look at tips to help prevent & manage constipation in the elderly with dementia.