Over a year ago, my mum, who’s living with Alzheimer’s, began showing signs of dysphagia. It started with a few harmless-sounding coughs after meals, but before long, every sip of water became a potential disaster waiting to happen. If you’ve never experienced that panic when your loved one struggles to swallow, consider yourself lucky. So, we did what anyone would do – we called in the experts: the Speech & Language Therapy Team.
Related: Spluttering Back to Life: A Personal Journey Navigating Dementia and Dysphagia
Six months later we had to call them again as mum’s condition worsened. They came to visit and assess mum again, with a new set of recommendations on how to navigate the next stages of dysphagia including moving us to Level 2 Liquids and Level 6 Foods.
This blog is a reflection on what we’ve learned as dysphagia worsened and some practical tips for other caregivers trying to keep their loved ones safe, happy, and well-fed while managing dysphagia.
(Note: This is not medical advice, I urge you to consult your own medical practitioners)

What is Dysphagia?
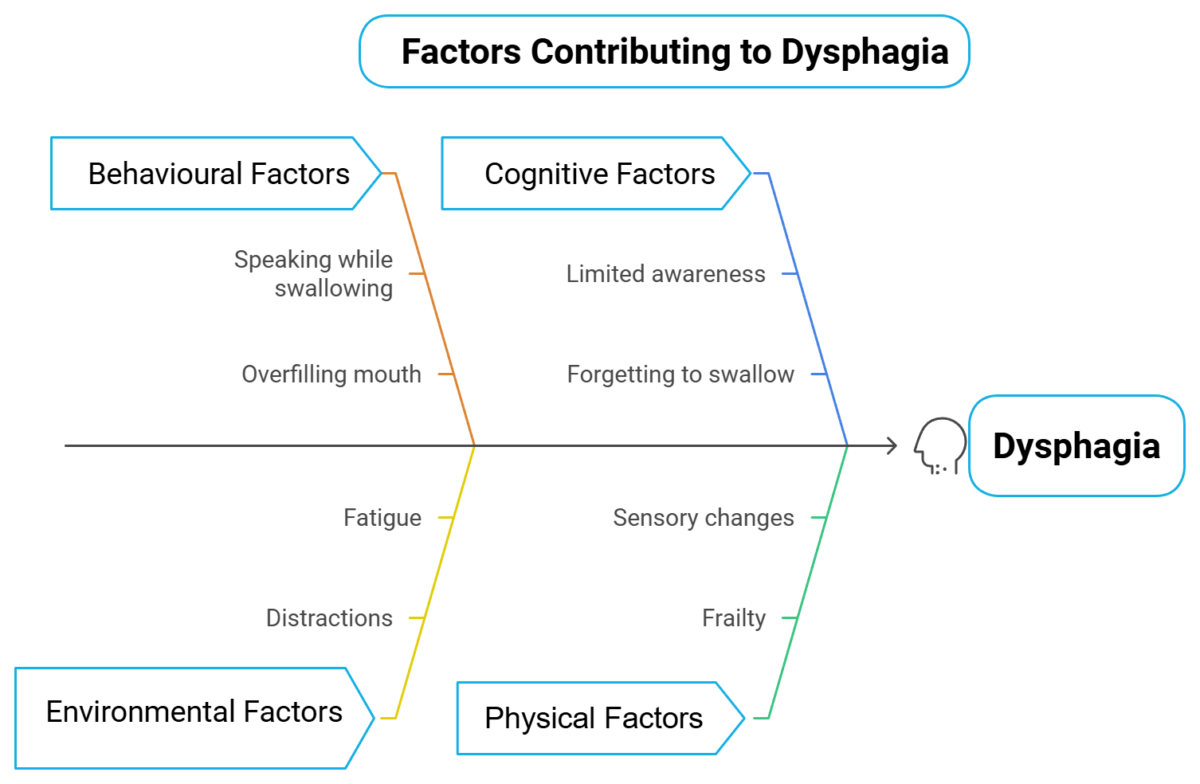
Did you know there are three types of dysphagia? That’s right, as if managing one wasn’t enough. At its core, dysphagia is a condition where swallowing becomes difficult or unsafe, that can lead to coughing, choking or aspirating on food or drink. Depending on where things go wrong, it falls into these categories:
- Oral Dysphagia: Trouble starts in the mouth. Think chewing & breaking down food becomes very difficult
- Oropharyngeal Dysphagia: The throat gets in on the action, making it hard to get food and drink past your windpipe.
- Esophageal Dysphagia: Food has a hard time reaching the stomach, so everything seems stuck mid-journey.
In mum’s case, it’s mostly a throat issue, thanks to the cognitive decline from her Alzheimer’s. But dysphagia can also happen due to other conditions like MS, Parkinson’s, or muscle weakness.

Enter the IDDSI Framework!
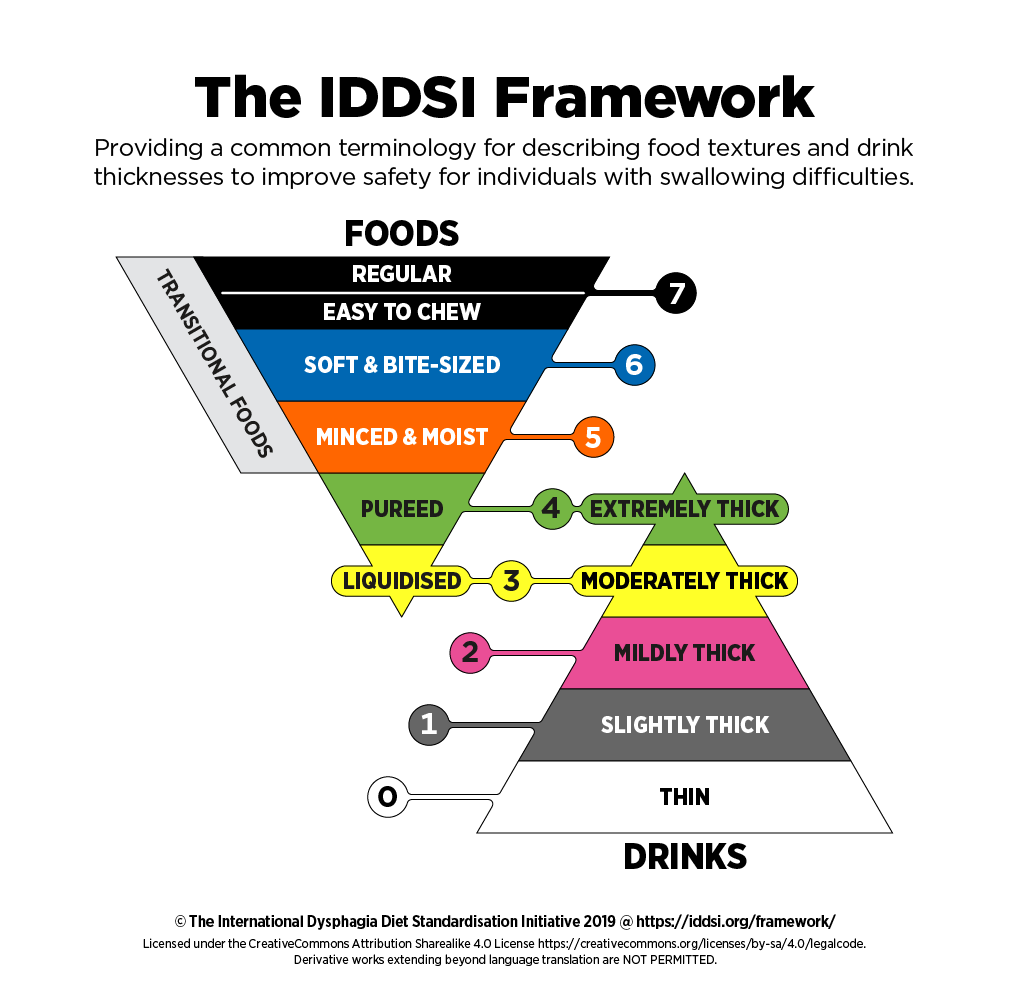
To help mum swallow safely, the Speech and Language therapist moved mum up the scale of the IDDSI framework. Sounds official, right? It’s like a Michelin star rating system, but for how mushy your food or how thick your drinks needs to be, it ranks foods and liquids on a scale from 0 (thin liquids like water) to 7 (normal, everyday foods). Here’s a quick breakdown:
We’ve been moved to Level 2 Liquids and Level 6 Foods.
- Level 2: Slightly thick liquids like a runny smoothie. Think drinking yoghurt, but a bit thicker to prevent choking.
- Level 6: Soft, bite-sized foods that don’t require much chewing, like mashed potatoes or soft veggies cut into little pieces.
It’s a globally recognised system that helps when talking about dysphagia and a common language helps as in the end it’s all about preventing choking hazards.
The New Normal: Adventures in Eating and Drinking
In addition to increased coughing and choking, a few things have stood out as the reason for mum’s transition to Level 2 liquids and Level 6 foods. Alzheimer’s already affects her memory, but now simple things like knowing when to swallow or not talking while eating have become foreign concepts. A few notable struggles:
- Forgetfulness: She forgets to swallow.
- Overstuffing: She takes huge mouthfuls or big sips, it became ‘the how much can I fit in my mouth at once’ challenge.
- Fatigue: Mid-meal naps have become a thing.
- Distraction: Try keeping focus at mealtime when you’re not interested at all
Each meal was full of tension, taking a spoonful of food or sip of a drink and waiting…….. would it result in a coughing fit?
Tips to Manage Dysphagia (Or, Things We Wish We Knew Sooner)
Here’s what we’ve learned at this stage of dysphagia that’s actually made a difference:
- Get Professional Help: The Speech & Language Therapy team is your best friend here. They’ll give you a plan and adjust as needed.
- Thicken Liquids: Yes, thickeners taste about as exciting as you’d imagine, but they’re lifesavers. Get them from your doctor, they’re specialist products!
- Supervise Everything: Full-time supervision during meals is non-negotiable at this point.
- Moist Food Is Your Friend: Add sauces, custards, or creams wherever possible. Dry food is the enemy. Funnily, fish fingers became a big issue, and we loved them!
- Avoid Tricky Foods: Juicy fruits, cereal with milk—anything with multiple textures is a no-go. Baked beans are off the menu because of skin separation, oh no!
- Hand-Under-Hand Support: This is a great trick to help with eating without taking away independence completely.
- Upright Position: Ensure mum’s sitting upright before, during, and for at least 30 minutes after meals.
- Eat Slowly: Small sips, tiny bites—no speed-eating contests here.
- Empty Mouth: Ensure the oral cavity is clear post eating and drinking
- Fatigue: Ensure fully alert when eating and drinking, stop if showing signs of fatigue
- Calm Environment: Turn off the TV, minimise distractions, and make the mealtime environment as peaceful as possible.
- Use Adaptive Tools: Special plates, cups, and cutlery can make a world of difference to increase focus.
- Measure your cup: this was a duh moment, we changed cups and had been adding the same amount of scoops to a cup that carried more liquid volume. The thickener became ineffective at slowing down liquid consumption when it was soooo thin, so measure your cup and adjust your scoops!
Related: Managing Dysphagia Alzheimer’s Caregiver Tips
We also had to manage another challenge: oral secretions. There were times it sounded like mum was drowning in her own saliva. Thanks to the Speech & Language team, we got a referral back to the doctor for medications that helped reduce this terrifying sound, a really scary time that I’m so glad has been resolved
Conclusion
If there’s one thing I’ve learned through this journey, it’s that every mealtime is a learning experience. Yes, dysphagia has made eating a challenge, but with the right tools, strategies, and plenty of patience, it’s manageable.
I know this isn’t the last hurdle we’ll face with mum’s Alzheimer’s and dysphagia and things will likely worsen again. But thanks to the Speech & Language Therapy team, I feel more prepared for whatever comes next. There’s less panic now, and I’m learning to take it all one day at a time.d If you’re a caregiver dealing with this, know that you’re not alone, and with the right support, you’ll figure it out too!



Thank you for this information. We haven’t reached this stage yet thankfully but it’s good to be prepared. In recent weeks my my sister’s appetite has waned. I take her a little picnic when I visit, small sandwiches, cheese and biscuits,pork pie, sausage rolls,little salads and crisps,but lately she has not eaten very much. Your article has made me think differently about wet and dry foods to offer her so thank you again for this information.
Thank you Pat. I’m glad it helped, consistency of food is definitely important for dysphagia, but I totally get the lack of interest, mum was the same for a while. Keep trying, look at use at colourful plates (contrasting to food colour), little an often also helps and reduce distractions. Eating together also helps, mum use to mimic me when she wasn’t eating particularly well, treats help as well! Good luck, if you do get to this stage always talk to your medical team who will have a speech therapy team who can advise. Good luck
When you are in long term care homes in Canada, there are Registered Dietitians on staff that are experts in dysphoria. They can be consulted at Assisted living facilities as well. This was not mentioned in this posting. SLPs are also on call for dementia but there are fewer of them around. The RD can call in the SLP on referral as well.
Thanks Kate, for clarifying the situation in Canada. I suspect its the same in many countries, with care homes having dietitians to help with food requirements and being able to call on SLP (Speech & Language Pathologist?). Appreciate you reading the blog and sharing this information.